___________________________________________________________________
Pryles (1958) reported that Staphylococcus aureus is a bacterium that has the ability to evolve and develop resistance to antibiotics in wide use.1 Jevons (1961) confirmed this finding.2 Curran (1980) reported S. aureus produces a tissue-destroying exotoxin.3 After six decades of antibiotic use, forms of S. aureus have evolved that are resistant to most common antibiotics, and this has become an important public health problem.4 These are given the name "methicillin-resistant Staphylococcus aureus" (MRSA). MRSA was once found primarily in hospitals, but new strains have entered the community.4 These new strains have acquired several new virulence factors.4 The existence of these virulent antibiotic-resistant pathogens pose serious problems for clinical management of infected patients.4
Recent reports indicate that community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) now has reached epidemic proportions in many areas and has become a worldwide problem.4-12 Kuehnert et al. (2006) estimate, based on samples obtained in the National Health and Nutrition Examination Survey, that 32.4 percent of the U.S. population are colonized with S. aureus.13 Circumcision long has been known to increase the risk of S. aureus infection in newborn boys. The advent of epidemic CA-MRSA dramatically worsens the risks associated with Staphylococcus infection because:
- the presence of CA-MRSA in epidemic proportions increases the chance of an infant being infected with MRSA by caregivers.
- the threat to health is escalated beyond that posed by methicillin-sensitive Staphylococcus aureus (MSSA) if an infant should be infected.
- the risk of death is increased.
This statement reviews the literature regarding MRSA with an emphasis on the risk to newborn circumcised boys.
The Circumcision Wound as Portal-of-Entry for Staphylococcus aureus
The circumcision wound is a known portal-of-entry for the pathogen and significantly increases circumcised boys' risk. Sauer (1943) reported fatal Staphylococcus broncho-pneumonia after ritual circumcision.14 Isbester (1959) identified circumcision as a factor in lowering resistance.15 Thompson et al. (1963,1965) reported that boys have about twice the infection rate of girls, and circumcised boys have twice as much SA disease as non-circumcised boys (26 percent compared to 13 percent).16,17 Kirpatrick & Eitzman (1974) reported a case of staphylococcal septicemia after neonatal circumcision.18 Annunziato & Goldblum (1978) reported staphylococcal scalded skin syndrome (SSSS) from infected circumcisions.19 Woodside (1980) reported a case of staphylococcal necrotizing fasciitis after "routine" non-therapeutic circumcision.20,21 Curran & Al-Salihi (1980) reported that male newborns have 5.5 times as much general exfoliative disease (SSSS) as girls.3 Enzenauer et al. (1985) reported the incidence of Staphylococcus aureus (SA) infection on follow-up among the circumcised males to be more than twice as high as among the non-circumcised males and 4 times higher than females.22 Stranko et al. (1986) reported staphylococcal impetigo in newborn circumcised males.23 Bliss et al. (1997) reported two cases of staphylococcal necrotizing fasciitis after circumcision.24 Boys already are at greater risk of SA infection than girls and neonatal circumcision worsens that disadvantage.3, 14,17,20-24
 Initial presentation of post-circumcision staphylococcal necrotizing fasciitis 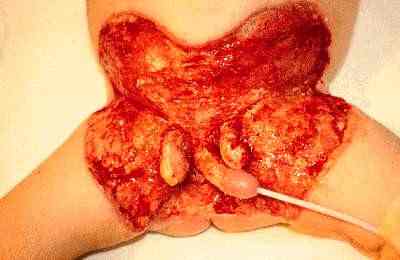 Patient after surgical debridement of infected tissue |
Transmission of Infection
The strictest aseptic surgical technique may not prevent infection of the circumcision wound with SA because the circumcision wound may be infected while the infant patient is in the newborn nursery or in the community after leaving the hospital. SA spreads rapidly through hospital nurseries and newborn boys quickly become colonized with SA.1,3,9,17,22-30 Infection frequently affects the diaper and groin area.16,22,29 Gooch & Brit (1978) reported that 24 percent of newborns are colonized at time of discharge and, of these, 2 percent have an infection.29 Enzenauer et al. (1984) commented, "Circumcision, by its very nature, requires more staff-person 'hands-on' contact, both during the procedure and during preoperative and postoperative care," so circumcised boys are more likely to be infected.30 Boys may also become infected in the home environment after leaving the hospital.28,31
Previous Nursery Outbreaks
There are numerous reports of outbreaks of SA among circumcised boys in hospital nurseries. Remington & Klein reported 25 outbreaks from 1961 to 1987 in U.S. hospital nurseries.32 Zafar et al. (1995) reported an outbreak of MRSA in a Virginia nursery.33 Hoffman et al. (2000) reported an outbreak of erythromycin-resistant methicillin sensitive Staphylococcus aureus among circumcised boys in a newborn nursery in North Carolina.34 Rabin (2003) reported an outbreak of MRSA among circumcised boys in the St. Catherine’s Hospital nursery on Long Island.35 Saiman et al. (2003) reported the outbreak of MRSA in a New York City newborn nursery.36 Nabiar et al. (2003) reported the outbreak of MRSA in a Washington, DC, newborn intensive care unit with one death.37 Bratu et al. (2005) reported an outbreak of MRSA in the nursery of a New York City hospital and said "the introduction of CA-MRSA strains into neonatal units represents an especially serious challenge."38
Bratu et al. (2005) identify surgical operations as a risk factor for MRSA infection in the newborn.38 Other researchers identify male neonatal circumcision as a specific risk factor.39,40 Nguyen et al. (2007) report that circumcised newborn boys are twelve times more likely to get a MRSA infection than a non-circumcised boy.40
Manifestations of Infection with MRSA
Some strains of MRSA produce fulminant infection that may progress rapidly to death.4 Isaacs et al. (2004) report that osteomyelitis and/or septic arthritis occurs in connection with MSSA, but more skin infection and cellulitis occurs in connection with MRSA.9 Zetola et al. (2005) report more outbreaks of skin infections, including epidemic furunculosis with possible septic shock, and cases of severe invasive pulmonary infections, including necrotizing pneumonia, in young, otherwise healthy people.4
In a paper presented to the American Academy of Pediatrics describing the effects of methicillin-resistant Staphylococcus aureus (MRSA) in newborns, Fortunov et al. (2005) report heavy outbreaks of pustulosis in the diaper area along with invasive infections including bacteremia, urinary tract infection, musculoskeletal infections, and empyema (pus in a body cavity).31 Fortunov et al. report MRSA in boys peaks at 7-12 days of age, which would be 6-11 days after non-therapeutic neonatal circumcision.31 The incubation period reported by Fortunov et al.31 is similar to that reported by Cohen (1992) for post-circumcision urinary tract infections.41 No peak was observed in girls.11 Boys had 73 percent of all infections.31 Ten of 12 invasive infections were in boys.31
MRSA is causing new and previously unknown diseases in infants and young children. Kikuchi et al. (2003) reported a new disease called neonatal toxic shock syndrome-like exanthematous disease (NTED).40 Adem et al. (2005) report three fatal cases of staphylococcal Waterhouse–Friderichsen Syndrome in young girls.43
Mortality
Staphylococcus aureus infection was often fatal in the pre-antibiotic era.44 If the SA is methicillin-resistant, mortality increases,4,5,45,46 and death is a possible outcome of MRSA infection. Pryles (1958) reported nine deaths among 24 infants with staphylococcal pneumonia for a mortality rate of 37.5%.1 Thompson et al. (1963,1965) report a higher mortality rate for males.16,17 Fortunov et al. (2005) report one male infant death.31 The CDC (1999) reports four pediatric deaths in North Dakota and Minnesota.45 Isaacs et al. (2004) report a mortality rate of 24.6 percent for MRSA-infected newborn babies as compared with 9.9 percent for MSSA-infected babies.9 Healy et al. (2004) report a mortality rate of 38 percent among MRSA infected newborn infants.46 Vince (2004) reports 800 deaths a year from MRSA in England and Wales.47 Noskin et al. (2005) report 12,000 inpatient deaths a year in U.S. hospitals caused by MRSA.50 According to Noskin et al., a patient with MRSA infection is five times more likely to die in hospital.50 Templeton (2005) reported that, at Great St. Ormond Street Hospital in England, out of 20 children with MRSA infection aged three-years or younger, four died, including one boy, born healthy, who died from MRSA infection 36 hours after birth,51 for a mortality rate of 20 percent.
Costs
Noskin et al. (2005), using data from the National Inpatient Survey, reports that the hospital stay and costs for adult patients triple when the patient has a MRSA infection.50 No data are available for infant or child patients.
Epidemiology
MRSA infection is an emerging epidemic disease. MRSA infection is not a reportable disease, consequently, epidemiological data have not been collected.
Outmoded Medical Society Statements.
Circumcision policy statements by medical societies do not consider the impact of epidemic MRSA, so their recommendations are no longer appropriate.52-56 In fact, the American Academy of Pediatrics has issued no statement to its members on the treatment of MRSA.
Even though a recent cost-utility study did not consider the advent of MRSA, it still found non-circumcision to be the better choice for optimum health and well-being.57 Non-circumcision was the preferred medical choice prior to the arrival of MRSA in epidemic proportions,52 56 57 and is even more so today. The advent of MRSA in epidemic proportions increases risks associated with male neonatal circumcision beyond those previously contemplated and further increases the desirability of the non-circumcision option.
MRSA and other antibiotic-resistant varieties of SA, such as vancomycin-resistant Staphylococcus aureus (VRSA), increase risk, including death, to newborn circumcised boys.4,31,43,44 In view of this increased risk, the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists should terminate their policy, most recently affirmed in 2002,58 of offering elective medically-unnecessary non-therapeutic neonatal circumcision at parental request.
Management of MRSA infection
Bliss et al. (1997) recommend early diagnosis, followed by rapid and aggressive treatment for a successful outcome.24 Professors Bamberger & Boyd (2005) provide a recent guidance on treatment.59 Kaplan (2005) also discusses treatment options.60 Mortality remains high even with the best treatment.59
Action Required
Doctors Opposing Circumcision consistently has advised parents that genital integrity (non-circumcision) is most likely to produce the highest state of health and well-being56,57 and is the preferred medical option for newborn boys.61 The arrival of community MRSA in epidemic proportions adds additional force to that recommendation.
Public health officials should act to suspend the performance of medically-unnecessary non-therapeutic circumcision of boys.
Hospital administrators must respond to this new threat to all newborn infants and especially circumcised male infants by limiting circumcisions to those for which there is a clear and present immediate medical indication and by increasing aseptic protocols in newborn nurseries.
Medical practitioners must consider the epidemic status of MRSA and exercise their independent judgment regarding the performance of non-therapeutic neonatal circumcision. There is an ethical duty to decline and avoid scientifically invalid treatment, especially when it puts the patient at risk.60 Doctors must act in the best interests of their child-patients regardless of parental requests.63-65 Doctors may conscientiously object to the performance of non-therapeutic circumcision of children.64-66
References:
- Pryles CV. Staphylococcal pneumonia in infancy and childhood. Pediatrics 1958:21(4):609-23. [Abstract]
- Jevons MP. "Celbenin"-resistant staphylococci. BMJ 1961;1:124-5.
- Curran JP, Al-Salihi FL. Neonatal staphylococcal scalded skin syndrome: massive outbreak due to an unusual phage type. Pediatrics 1980;66(2):285-90. [Full Text]
- Zetola N, Francis JS, Nuermberger EL, Bishai WR. Community-acquired meticillin-resistant Staphylococcus aureus: an emerging threat. Lancet Infect Dis 2005;5(5):275-86. [Full Text]
- Andrew E. Simor, Marianna Ofner-Agostini, Elizabeth Bryce, et al. The evolution of methicillin-resistant Staphylococcus aureus in Canadian hospitals: 5 years of national surveillance. Can Med Assoc J 2001;165:21-6. [Full Text]
- Khairulddin N, Bishop L, Lamagni TL, et al. Emergence of methicillin resistant Staphylococcus aureus (MRSA) bacteraemia among children in England and Wales, 1990-2001. Arch Dis Child 2004; 89:378-9. [Full Text]
- Gray JW. MRSA: the problem reaches paediatrics. Arch Dis Child 2004;89:297-8. [Full Text]
- Dietrich DW, Auld DB, Mermel LA. Community-Acquired methicillin-resistant Staphylococcus aureus in Southern New England children. Pediatrics 2004;113: e347 - e352. [Full Text]
- Isaacs D, Fraser S, Hogg G, Li HY. Staphylococcus aureus infections in Australasian neonatal nurseries Arch Dis Child Fetal Neonatal Ed 2004;89:F331-5. [Full Text]
- Kaplan SL, Hulten KG, Gonzalez BE, et al. Three-year surveillance of community-acquired Staphylococcus aureus infections in children. Clin Infect Dis 2005;40(12);1785-91. [Abstract]
- Gonzalez BE, Martinez-Aguilar G, Kristina G. Hulten KG, et al. Severe staphylococcal sepsis in adolescents in the era of community-acquired Methicillin-resistant Staphylococcus aureus. Pediatrics 2005;115(3):642-64.[Abstract]
- Purcell K, Fergie J. Epidemic of community-acquired methicillin-resistant Staphylococcus aureus infections: A 14-year study at Driscoll Children’s Hospital. Arch Pediatr Adolesc Med 2005;159:980-5. [Abstract]
- Kuehnert MJ, Kruszon-Moran D, Hill HA, et al. Prevalence of Staphylococcus aureus nasal colonization in the United States, 2001-2002. J Infect Dis 2006;193(2):172-9. [Medline]
- Sauer LW. Fatal staphylococcus bronchopneumonia following ritual circumcision. Am J Obstetr Gynecol 1943;46:583. [Full Text]
- Isbister C. Staphylococcal infection in infancy. Med J Aust 1959;2:629-33.
- Thompson DJ, Gezon HM, Hatch TF, et al. Sex distribution of Staphylococcus aureus colonization and disease in newborn infants. New Engl J Med 1963:269;337-41.
- Thompson DJ, Gezon HM, Rogers KD, et al. Excess risk of staphylococcus infection and disease in newborn males. Am J Epidemiol 1965;84(2):314-28. [Abstract]
- Kirkpatrick BV, Eitzman DV. Neonatal septicemia after circumcision. Clin Pediatr 1971;13(9):767-8. [Full Text]
- Annunziato D, Goldblum LM. Staphylococcal scalded skin syndrome. A complication of circumcision. Am J Dis Child 1978;132(12):1187-8. [Full Text]
- Woodside JR. Necrotizing fasciitis after neonatal circumcision. Am J Dis Child 1980;134(3):301-2. [Full Text]
- Woodside JR. Circumcision disasters. Pediatrics 1980;65:1053-54. [Full Text]
- Enzenauer RW, Dotson CR, Leonard T, et al. Male predominance in persistent staphylococcal colonization and infection of the newborn. Hawaii Med J 1985;44(10):389-90, 392, 394-6. [Full Text]
- Stranko J, Ryan ME, Bowman AN. Impetigo in newborn male infants associated with a plastic bell circumcision. Pediatr Infect Dis 1986;5(5):597-9. [Full Text]
- Bliss Jr DP. Healey PJ, Waldhausen JHT. Necrotizing fasciitis after Plastibell circumcision. J Pediatr 1997;31:459-462. [Full Text]
- Cook J, Parish JA, Shooter RA: Acquisition of Staphylococcus aureus by newborn babies in a hospital maternity department. Br Med J 1938;1:74-8.
- Gillespie WA, Simpson K, Tozer RC. Staphylococcal infection in a maternity hospital. Lancet 1959;2:1075-80.
- Hurst V. Transmission of hospital staphylococci among newborn infants. Pediatrics 1960;25:204-14. [Abstract]
- Payne MC, Wood HF, Karakawa W, Gluck L. A prospective study of staphylococcal colonization and infections in newborns and their families. Am J Epidemiol 1966:82:305-16.
- Gooch JJ, Britt EM. Staphylococcus aureus colonization and infection in newborn nursery patients. Arch Pediatr Adolesc Med 1978;132(9):893-6. [Abstract]
- Enzenauer RW, Dotson CR, Leonard T, et al. Increased incidence of neonatal staphylococcal pyoderma in males. Mil Med 1984:149:408-10.
- Fortunov RM, Hulten KG, Hammerman WA, et al. Community-acquired Staphylococcus aureus infections in term and near term previously healthy neonates. Presented at American Academy of Pediatrics Annual Conference, Washington, DC, Sunday, October 8, 2005.
- Remington JS, Klein JO. Infectious diseases of the fetus and newborn infant. 3rd ed. Philadelphia: WB Saunders, 1990:1001-3.
- Zafar AB, Butler RC, Reese DJ, et al. Use of 0.3% triclosan (Bacti-Stat) to eradicate an outbreak of methicillin-resistant Staphylococcus aureus in a neonatal nursery. Am J Infect Control 1995;23(3):200-8. [Abstract]
- Hoffman KK, Weber DJ, Bost R, Rutala WA. Neonatal Staphylococcus aureus pustulous rash outbreak linked by molecular typing to colonized healthcare workers. Presented at Centers for Disease Control and Prevention 4th Decennial International Conference on Nosocomial and Healthcare-Associated Infections. Atlanta, Georgia, March 5-9, 2000. [Abstract]
- Rabin R. Mysterious crop of staph: newborns, moms infected after stay at St. Catherine. Newsday, Long Island, New York, October 9, 2003. [Full Text]
- Saiman L, Cronquist A, Wu F, et al. An outbreak of methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit. Infect Control Hosp Epidemiol 2003; 24:317-21. [Medline]
- Nambiar S, Herwaldt LA, Singh N. Outbreak of invasive disease caused by methicillin-resistant Staphylococcus aureus in neonates and prevalence in the neonatal intensive care unit. Pediatr Crit Care Med 2003;4(2):220-6. [Medline]
- Bratu S, Eramo A, Kopec R, et al. Community-associated methicillin-resistant Staphylococcus aureus in hospital nursery and maternity units. Emerg Infect Dis 2005,11(6): Available from http://www.cdc.gov/ncidod/EID/vol11no06/04-0885.htm [Full Text]
- Van Howe RS, Robson WLM. The possible role of circumcision in newborn outbreaks of community-associated methicillin-resistant Staphylococcal aureus. Clin Pediatr 2007;46(4):356-8. [Full Text]
- Nguyen DM, Bancroft E, Mascola L, et al. Risk factors for neonatal methicillin-resistant Staphylococcus aureus infection in a well-infant nursery. Infect Control Hosp Epidemiol 2007;28(4):406-11. [Full Text]
- Cohen HA, Drucker MM, Vainer S, et al. Postcircumcision urinary tract infection. Clin Pediatr 1992;31(6):322-4. [Medline]
- Kikuchi K, Takahashi N, Piao C, et al. Molecular epidemiology of methicillin-resistant Staphylococcus aureus strains causing neonatal toxic shock syndrome-like exanthematous disease in neonatal and perinatal wards. J Clin Microbiol 2003;41(7):3001-6. [Full Text].
- Adem PV, Montgomery CP, Husain AN, et al. Staphylococcus aureus sepsis and the Waterhouse-Friderichsen syndrome in children. N Engl J Med 2005;353:1245-51. [Summary]
- Skinner D, Keefer CS. Significance of bacteremia caused by Staphylococcus aureus. Arch Intern Med 1941;68:851-75.
- Engemann JJ, Carmeli Y, Cosgrove SE, et al. Adverse clinical and economic outcomes attributable to methicillin resistance among patients with Staphylococcus aureus surgical site infection. Clin Infect Dis 2003;36(5):592-8. [Medline]
- Cosgrove SE, Sakoulas G, Perencevich EN, et al. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia; a meta-analysis. Clin Infect Dis 2003;36:53-9. [Medline]
- Centers for Disease Control and Prevention. Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus—Minnesota and North Dakota, 1997-1999. MMWR Morb Mortal Wkly Rep 1999;48(32):707-10. [Full Text]
- Healy CM, Hulten KG, Palazzi DL, et al. Emergence of new strains of methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit. Clin Infect Dis 2004;39:1460-6. [Medline]
- Vince G. MRSA deaths up 15-fold in a decade. New Scientist, London, February 26, 2004. [Full Text]
- Noskin GA, Rubin RJ, Schentag JJ, et al. The burden of Staphylococcus aureus infections on hospitals in the United States: an analysis of the 2000 and 2001 Nationwide Inpatient Sample Database. Arch Intern Med 2005;165:1756-61. [Abstract]
- Templeton SK. Hidden infant toll of MRSA. Sunday Times, London, April 10, 2005. [Full Text]
- Fetus and Newborn Committee, Canadian Paediatric Society. Neonatal circumcision revisited. Can Med Assoc J 1996; 154(6): 769-80. [Full Text]
- American Academy of Pediatrics Task Force on Circumcision. Circumcision Policy Statement. Pediatrics 1999;103(3):686-93. [Full Text]
- Council on Scientific Affairs. Report 10: Neonatal circumcision. Chicago: American Medical Association, 1999. [Full Text]
- AAFP Commission on Clinical Policies and Research. Position Paper on Neonatal Circumcision. Leawood, Kansas: American Academy of Family Physicians, 2002. [Full Text]
- Beasley S, Darlow B, Craig J, et al. Position statement on circumcision. Sydney: Royal Australasian College of Physicians, 2004. [Full Text]
- Van Howe RS. A cost-utility analysis of neonatal circumcision. Med Decis Making 2004;24:584-601. [Abstract]
- American Academy of Pediatrics, American College of Obstetricians and Gynecologists. Guidelines for Perinatal Care, Fifth Edition, November 2002: p.111.
- Bamberger DM, Boyd SE. Management of Staphylococcus aureus infections. Am Fam Physician 2005;72(12):2474-81. [Full Text]
- Kaplan SL. Treatment of community-associated methicillin-resistant Staphylococcus aureus infections. Pediatr Infect Dis J 2005;24(5:):457-8.
- Spilsbury K, Semmons JB, Wisniewski ZS, Holman CD. Routine circumcision practice in Western Australia. ANZ J Surg 2003;73(8):610-4. [Full Text]
- Opinion E8.20. Current opinions. In: Code of Medical Ethics, Chicago: American Medical Association, 1998. [Full Text]
- Committee on Bioethics, American Academy of Pediatrics. Informed consent, parental permission, and assent in pediatric practice. Pediatrics 1995;95(2):314-7. [Full Text]
- Committee on Medical Ethics. The law & ethics of male circumcision - guidance for doctors. London: British Medical Association, 2003. [Full Text]
- College of Physicians and Surgeons of British Columbia. Infant Male Circumcision. In: Resource Manual for Physicians. Vancouver, BC: College of Physicians and Surgeons of British Columbia, 2004. [Full Text]
- Denniston GC, Geisheker JV, Hill G. Conscientious Objection to the Performance of Circumcision of Children. Seattle: Doctors Opposing Circumcision, 2005. [Full Text]
Doctors Opposing Circumcision
Suite 42
2442 NW Market Street
Seattle, Washington 98107-4137
USA
Sunday, October 23, 2005.
(Revised Friday, December 2, 2005.)
(Revised Sunday, January 1, 2006.)
(Revised Sunday, January 21, 2006.)
(Revised Sunday, February 5, 2006.)
(Revised Saturday, February 11, 2006.)
(Revised Wednesday, March 8, 2006.)
(Revised Saturday, January, 12, 2008.)
No comments:
Post a Comment